The science of coronavirus: Your questions, answered
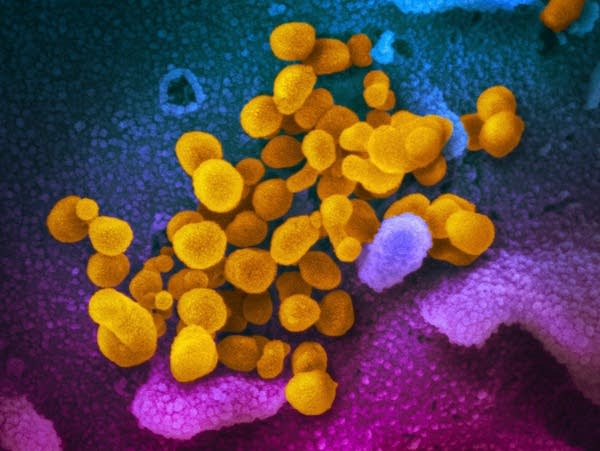
The novel coronavirus (yellow) emerge from the surface of cells (blue/pink) cultured in the lab. It's also known as 2019-nCoV, the virus causes COVID-19.
U.S. National Institutes of Health via AP file
Go Deeper.
Create an account or log in to save stories.
Like this?
Thanks for liking this story! We have added it to a list of your favorite stories.


